Kongresszusi összefoglaló / Congress review
Higlights from Gastro Update Europe 2019
Summary
This narrative review summarizes a selection of recent, clinically-important novel gastrointestinal developments, presented and discussed at the European Gastro Update In Budapest. The selected topics reflect what the distinguished faculty considered of vital importance to be communicated to the astute busy gastro-hep clinician, who is eager to stay well informed of important novel developments in his discipline. Whenever appropriate a personal comment or addition was added to further raise the educational value of this review. Given its narrative character, statements and conclusions are largely expert opinion-based and referencing is limited to the selected images.
Novel upper gastrointestinal developments
Prof Peter Malfertheiner
Gastro-esophageal reflux disease (GERD) may well be further increasing as H. Pylori infection risk continues to fall. Pathophysiological concepts, summarized in the figure below remain essentially unchanged (Fig. 1) but there is increasing interest in the concomitant role of functional dyspepsia with mucosal gastro-duodenal inflammation, delayed gastric emptying and impaired gastric accommodation, all favoring transient sphincter relaxations, together with enhanced sensitivity.
Figure 1. Pathophysiology of gastroesophageal reflux disease (1)
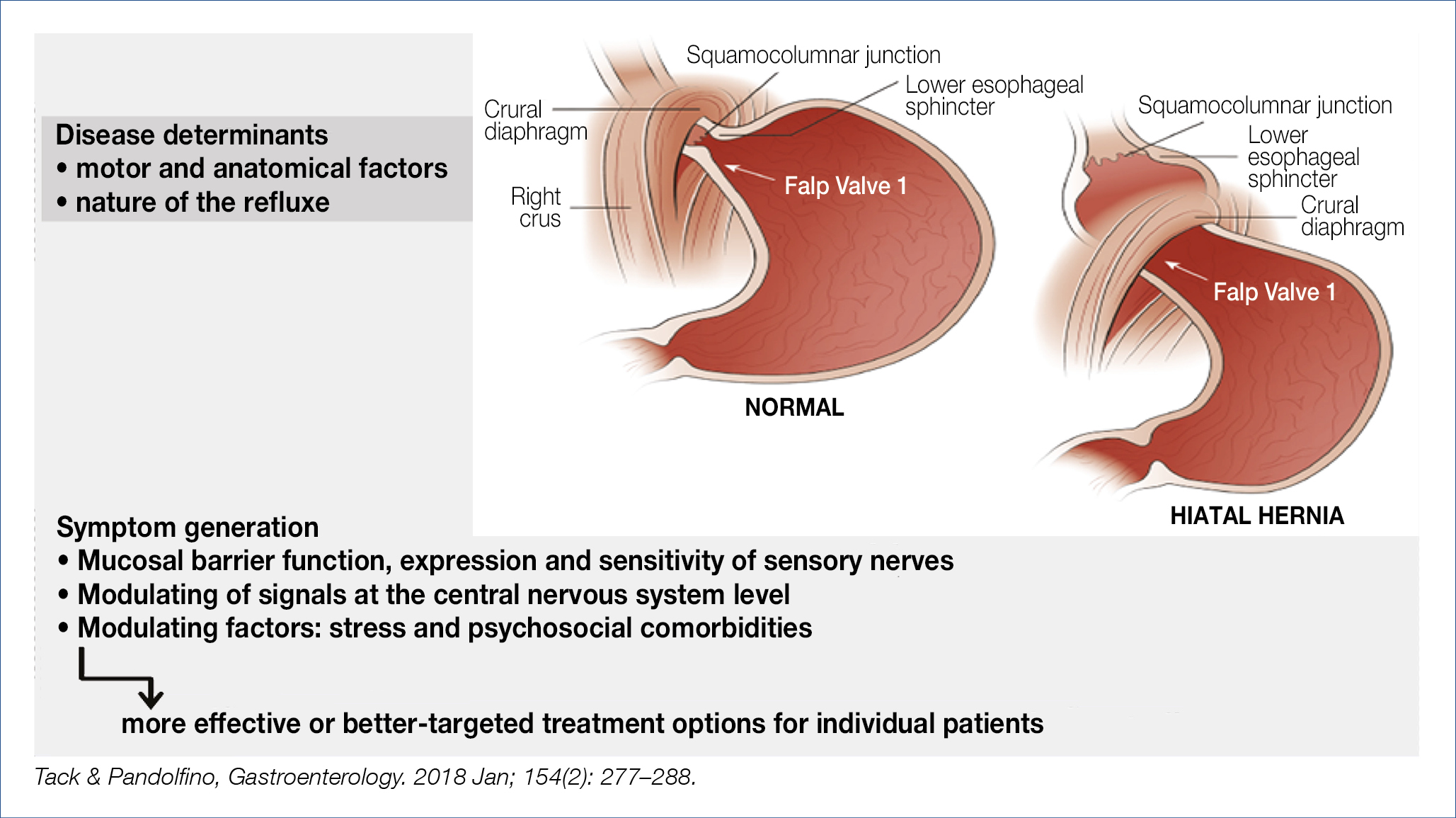
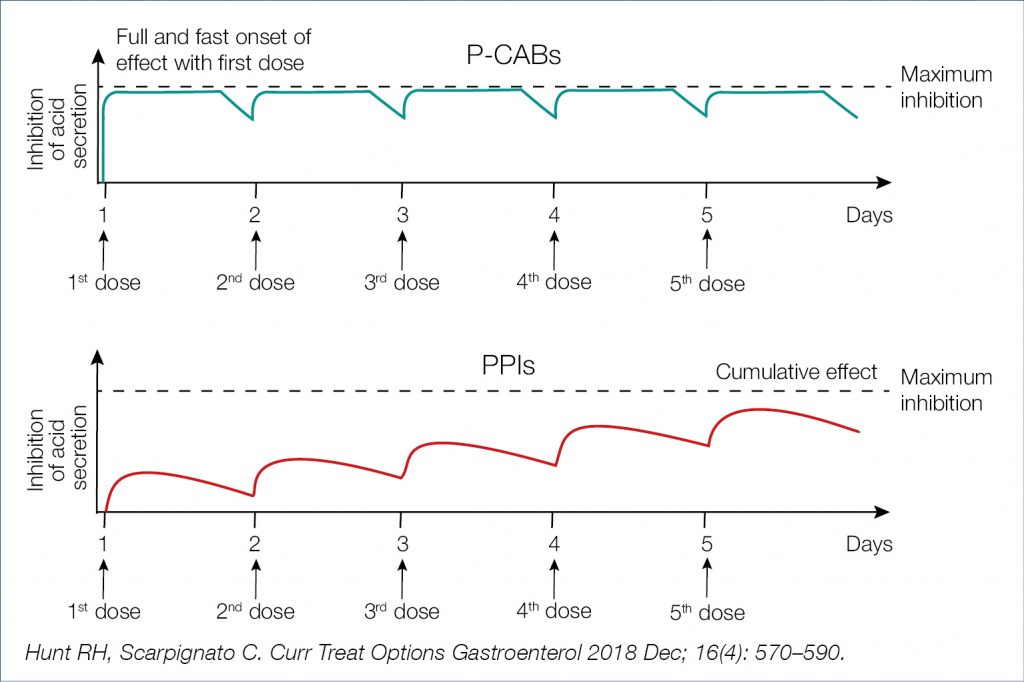
Hypersensitivity appears, in part, related to altered afferent signaling and aberrant sensory characteristics. Whereas infusion of menthol in the esophagus evoked a mild cold sensation in healthy subjects, this was perceived as rather painful heartburn in GERD patients. Refractoriness to proton pump inhibition (PPI) (esomeprazole 40 mg/d/8w) remains a challenging problem and deserves prolonged multichannel impedance-pH investigation. As shown in an Italian study, only one third of such patients had non-erosive reflux disease (+acid exposure time and +symptom association probability), the others suffered from reflux hypersensitivity (normal acid exposure time) or from functional heartburn. For those true non-responders, more profound acid suppression with a potassium-competitive acid blocker (pCAB) would be an option. As shown in the figures below, the mechanism of action of pCABs differs from that of PPIs (Fig. 2, Fig. 3). A recent Japanese study in PPI-refractory patients showed normalisation of esophageal acid exposure in 46%, together with symptom improvement and healing of esophagitis with 20 mg/d vonoprazan. For the time being pCABs are not (yet) available in Europe.
Figure 2. P-CABs (vonoprazan, revaprazan) and PPIs Main Differences in the Mechanism of Action (2)
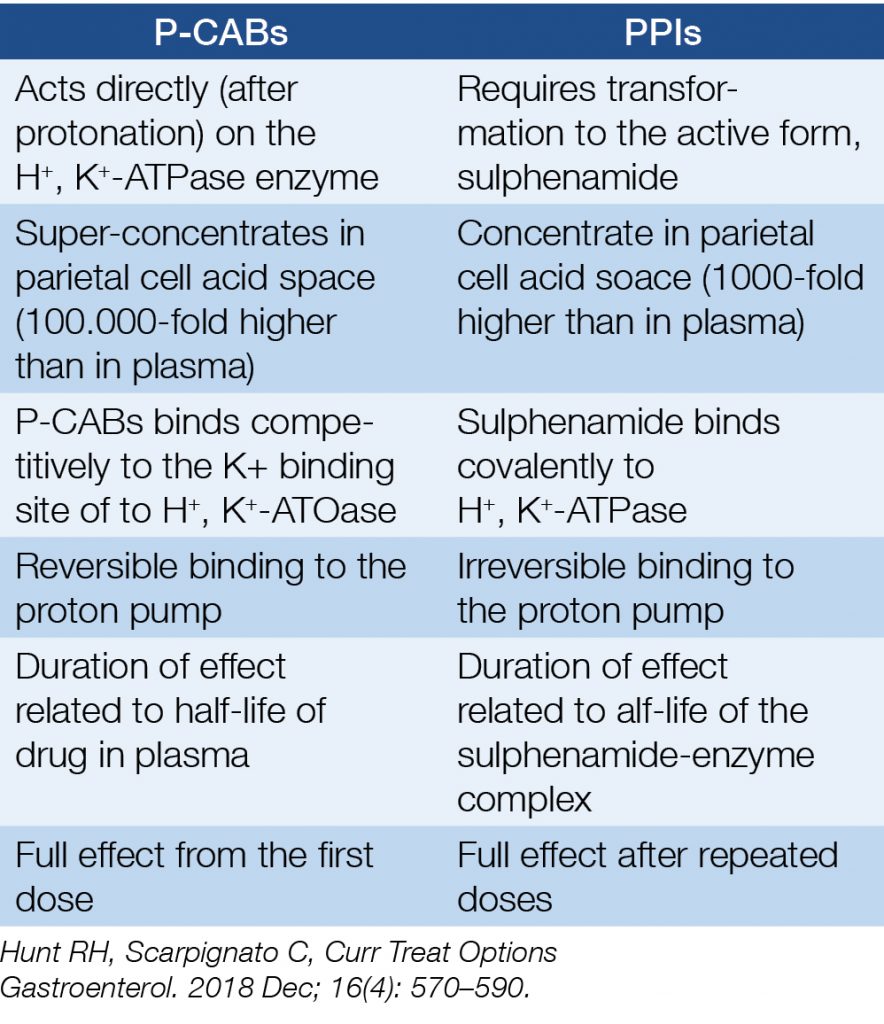
Figure 3. Time course of acid inhibition by P-CABs and PPIs: computer simulation (2)
Regurgitation, particularly when severe, may also be refractory even to high-dose PPI therapy and calls for other approaches, such as endoscopic fundoplication, magnetic sphincter augmentation, or standard antireflux surgery.
Esophageal columnar metaplasia (Barrett) continues to raise major clinical interest and controversy. Whether all patients with Barrett esophagus, also those that are asymptomatic should enter a surveillance program to detect early neoplasia, is not answered in a uniform way in the currently existing guidelines. It is also somewhat controversial whether acid suppression with PPIs decreases the cancer risk because PPIs are commonly prescribed for reduction of heartburn symptoms. In support of non-stop acid suppression was a recent nested case-control study in 300 American veterans showing a 41% reduction in esophageal adenocarcinoma in PPI users. Can chemoprevention be further improved by combining PPIs with aspirin? The long-awaited results of the large British AspECT chemoprevention study, which randomized 2,557 patients to low-(20 mg/d) or high-dose (40 mg × 2/d) esomeprazole with or without 300 mg aspirin/d, followed for a median 8.9 years, were recently published. High-dose PPI was superior to low-dose PPI in delaying the combined end point of [all-cause mortality, high-grade dysplasia or adenocarcinoma]. Aspirin was not significantly associated with a decreased risk of the combined outcome. It would appear that the benefit of the study was largely related to a reduction of all-cause mortality. What does this all mean for clinicians? For the time being clinicians should try to stratify patients in a low or high risk category using the common clinical/endoscopic characteristics. Low risk patients should be advised to stop smoking, moderate the diet and receive chemoprevention with (high dose) PPI and aspirin. High risk patients should enter an endoscopic surveillance program and be treated whenever dysplastic/neoplastic changes develop with endoscopic resection and/or radiofrequency ablation or other alternative modalities. Remember that it is not unusual that only about half of the clinicians adhere to established guidelines.
Inappropriate polypharmacy, especially in older people, imposes a substantial burden of adverse drug events, ill health, disability, hospitalization and even death. It was estimated that 30% of American elderly consumed 5–9 pills per day. PPIs, of which the consumption is still rising, were often included. When correctly prescribed PPIs play an essential therapeutic role in medicine. A recent high-quality systematic review and meta-analysis demonstrated the substantial benefits of PPI treatment. Over 140,000 patients were analysed in 580 prevention trials, 233 healing trials and 36 bleeding trials. Compared to controls and other gastro-protectants, PPIs were overall 5 times more effective in reducing risk and 5 times more effective in tissue improvement/healing. This glamorous result needs to be balanced with the negative consequences of long-term PPI induced acid suppression, particularly when related to enhanced esophageal and gastric cancer risk as discussed in last year’s highlight. Despite all critical comments and study shortcomings, it would seem sensible to add neoplasia to well-known list of adverse events, shown in the figure below (Fig. 4).
Figure 4. PPI and adverse events Ongoing debates (3)
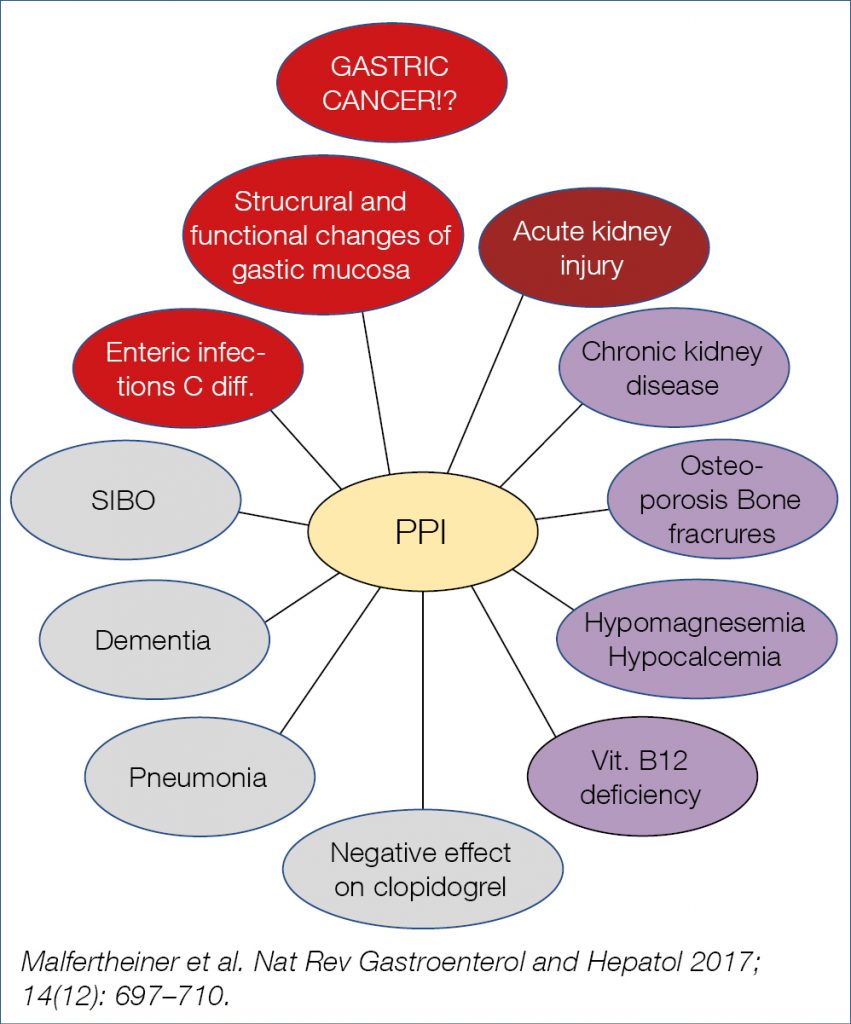
The enhanced gastric cancer risk of long-term acid suppression may well be related in part to gastric dysbiosis and perhaps to chronically elevated gastrin levels. Interestingly, in one study the enhanced risk was only seen in those individuals who were not taking additional Aspirin. Clinicians should be aware of the above-mentioned association studies, while realising that randomized controlled trials are impossible and that association studies are always prone to known and unknown confounders. Anyhow, the main message of all these studies is that chronic profound (PPI-induced) acid suppressant therapy should only be prescribed for the proper indications, realising that a very substantial percentage of PPI prescriptions, also in the elderly, are inappropriate.
Eosinophilic esophagitis prevalence is rising also in the Far East, becoming the leading cause of esophageal food impaction in children and young adults. The prevalence, calculated in 24 studies is now ~34/100.000. Note that a proper diagnosis does no longer require disease resistance to PPI therapy, as up to 60% of genuine eosinophilic esophagitis patients respond to PPIs, presumably based at least in part upon their anti-inflammatory activity. The terminology of PPI-responsive esophageal eosinophilia should therefore be omitted in clinical practice. The updated international consensus diagnostic criteria for eosinophilic esophagitis includes: – symptoms of esophageal dysfunction – at least 15 eosinophils per high-power field (~60/mm2) and – comprehensive exclusion of other disorders that could contribute to esophageal eosinophilia. The most important pathogenetic features are summarized in the figure below (Fig. 5).
Figure 5. Pathogenesis of eosinophilic esophagitis (4)
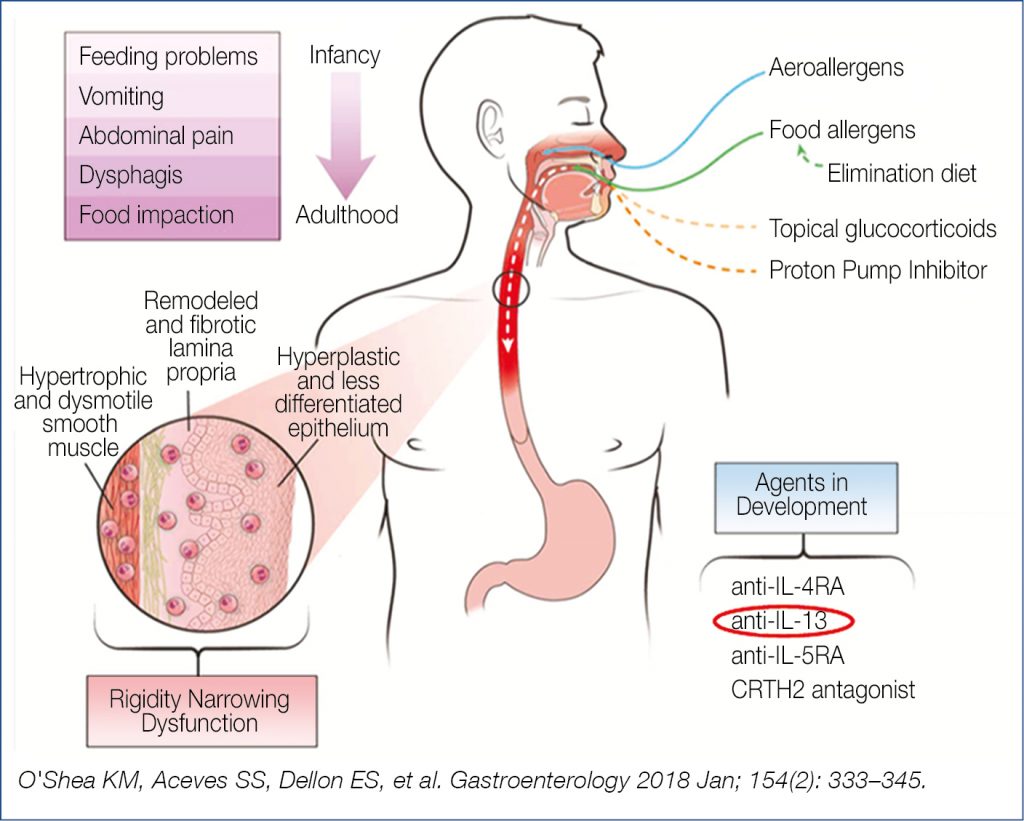
According to a systematic review, H. Pylori exposure was associated with a 37% reduction in the risk of eosinophilic esophagitis. This finding fits with the observation that exposure to H. Pylori early in life skews immune responsiveness more in the T helper 1 direction than in the pro-allergy T helper 2 direction. Medical therapy usually starts with PPIs, followed by corticosteroids if PPIs fail. A recent 8 week controlled trial comparing oral viscous budesonide with fluticasone inhalation revealed equal reduction in mucosal eosinophilia and improvement in dysphagia. Two important drivers of eosinophilic activation are IL-5 and IL-13. A monoclonal antibody targeting IL-5 has already been shown to be efficacious. Novel is the experimental evaluation of a monoclonal antibody against IL-13 which was also shown to be efficacious in reducing esophageal eosinophilia and in reducing symptomatology, deserving further evaluation. Not discussed at the meeting but important to mention is the renewed interest in empiric elimination diet to decrease the allergenic load. It all started with the step-down six-food elimination diet, followed by 4-food and the 2-food elimination diet (the 6-4-2 system) with the gradual re-introduction of nutrients, a costly time-consuming laborious procedure. A more rational, patient-friendlier approach, decreasing the endoscopic burden, was launched in Spain, the (2-4-6) step-up protocol, thus starting with the 2-food (milk, wheat) elimination diet (which was effective in ~40%, the majority related to avoidance of milk or dairy) with sequential elimination of other food items. Ultimately, there will be a sequence of eliminations: (dairy), (+wheat), (+egg), (+soy/legumes), (+nuts, seafood), (+beef/corn). In practice, successful dietary therapy demands substantial patient education, engagement and motivation to adhere to the elimination diet.
It is common knowledge that H. Pylori infection is associated with multiple gastroduodenal and extra-intestinal manifestations. In a recent important meta-analysis the role of H. Pylori infection was evaluated in low-dose Aspirin users. In infected individuals, the risk of Aspirin-induced ulceration rose by almost 70% and in the absence of protective acid suppressants, by almost 100%. Low-dose Aspririn, variably defined in the literature is not innocent therapy. I wonder to what extent chronic low-dose Aspirin may be related to the common anemia seen in the elderly.
Most of the information of H. Pylori eradication in the prevention of gastric cancer was generated in the Far East. Now, also data from a western population became available. A population based cohort of over 95,000 individuals with eradication of the infection was followed; overall 0.1% developed gastric cancer. The risk decreased gradually with incidence ratios of 8.6 after 3-5 y and 0.3 after 5-7.5 y of follow-up, confirming the gradual suppression of gastric cancer development. Similar results were seen in asymptomatic individuals from a health screening program; compared to controls the risk of gastric cancer expressed as hazard ratio’s (HR) was 4.12 and dropped to 2.73 in those after H. Pylori eradication. One may readily assume that such cancer protective effect is related to the gradual improvement of atrophic gastritis and even (partial) reversibility of intestinal metaplasia after eradication of the infection. Such phenomenon may also explain the prevention of metachronous gastric cancer shown in a randomized trial of 470 patients after endoscopic removal of early gastric cancer. Metachronous cancer developed in 7% in the eradiation group versus 13% in the placebo group, again paralleled by improvement in atrophy in respectively 48% versus 15%. Despite some recent publications from the western world, it is still unclear whether population screening for H. Pylori infection and serologic screening for pre-neoplastic gastric mucosal atrophy/metaplasia is warranted. Should serologic screening be encouraged in combination with screening for colorectal neoplasia in individuals above 59 y in western societies that have low or intermediate risk of gastric cancer? Should fecal occult blood screening be combined with stool H.Pylori antigen screening?
The drama with the rising antimicrobial resistance, particularly for clarithromycin, metronidazole and levofloxacin continues. Successful therapies for infectious diseases should ideally be susceptibility-based but this involves extra costs and effort compared to empiric therapies. This dilemma was recently studied in a controlled trial involving 382 patients, randomized to 14 d empiric quadruple therapy (esomeprazole, bismuth, amoxicillin, metronidazole) versus susceptibility-guided therapy, with respective eradication rates per protocol of 97.6% versus 97.7% and per intention-to-treat of 85.4% versus 91.6, a non-significant difference. It remains difficult to recommend susceptibility-based treatment for first-line therapy in clinical practice until such therapy is proven to be superior and cost-effective. Perhaps all this will change if the initial remarkable eradication results with 14 d dual therapy with high-dose esomeprazole and amoxicillin can be reproduced in other cohorts in the west. The results mirror the high eradication also obtained with dual therapy with the pCAB vonoprazan and amoxicillin. It would certainly be progress if such dual therapy would be effective because resistance to amoxicillin is almost negligable; the only problem would be penicillin allergy.
Small bowel diseases and infections
Prof Gerhard Rogler
Celiac disease is thought to affect 1% of the western population. HLA haplotypes DQ2 and DQ8 are present in over 90% of the celiac patients compared to ~40% in the general population. Celiac disease may be associated with other autoimmune diseases. In addition to intestinal symptoms, celiac disease may be complicated by vitamin and trace mineral deficiencies, bone disease and malignancy. Non-celiac gluten intolerance/sensitivity and seronegative celiac disease have recently been described. Perhaps enterovirus infection may increase the risk of developing celiac disease. Monthly stool samples from Norwegian DQ2/DQ8 positive children were checked starting from age month 3 to 36 for enterovirus and adenovirus using RT-PCR. After a mean of ~10 y, celiac disease was diagnosed in 25 of 220 children. Enterovirus was found in 17% of the stool samples and was significantly more frequent in samples collected before development of celiac disease antibodies. Such data are quite intriguing and ask for more information to fully understand the way early viral infection leads to celiac enteropathy in predisposed individuals.
A meticulously followed gluten-free diet is so far the only treatment to antagonize the chronic inflammatory tissue destruction. An important recent study revealed that chronic inflammation permanently reconfigures the tissue-resident lymphocytic compartment. Normally there is a stable tissue-resident lymphocyte population which plays a key role in immune surveillance. In celiac disease, gluten-induced inflammation triggers a depletion of such naturally occurring intraepithelial lymphocytes. Exclusion of dietary gluten appears insufficient to reconstitute this important subset of intraepithelial lymphocytes. Clinicians should be aware of the extensive differential diagnosis in celiac-like mucosal abnormalities; conditions accompanied by enhanced intraepithelial lymphocytosis include: NSAID or PPI consumption, Giardia or Cryptosporidium infection, immunodeficiency disorders, bacterial overgrowth, IBS etc.; conditions accompanied by villus atrophy with or without intraepithelial lymphocytosis include: angiotensin receptor blocker-associated enteropathy (olmesartan etc.), mycophenolate mofetil, autoimmune enteropathy, immunodeficiency disorders, eosinophilic disorders, chemoradiation etc. Olmesartan-associated enteropathy is an under-diagnosed cause of diarrhea, weight loss and pan-malabsorption. Lifelong strict gluten-free diet therapy is demanding, which explains the many strategies for non-dietary treatment which are currently being explored as exemplified in the figure below (Fig. 6).
Figure 6. Current strategies for non-dietary treatment of celiac disease (5)
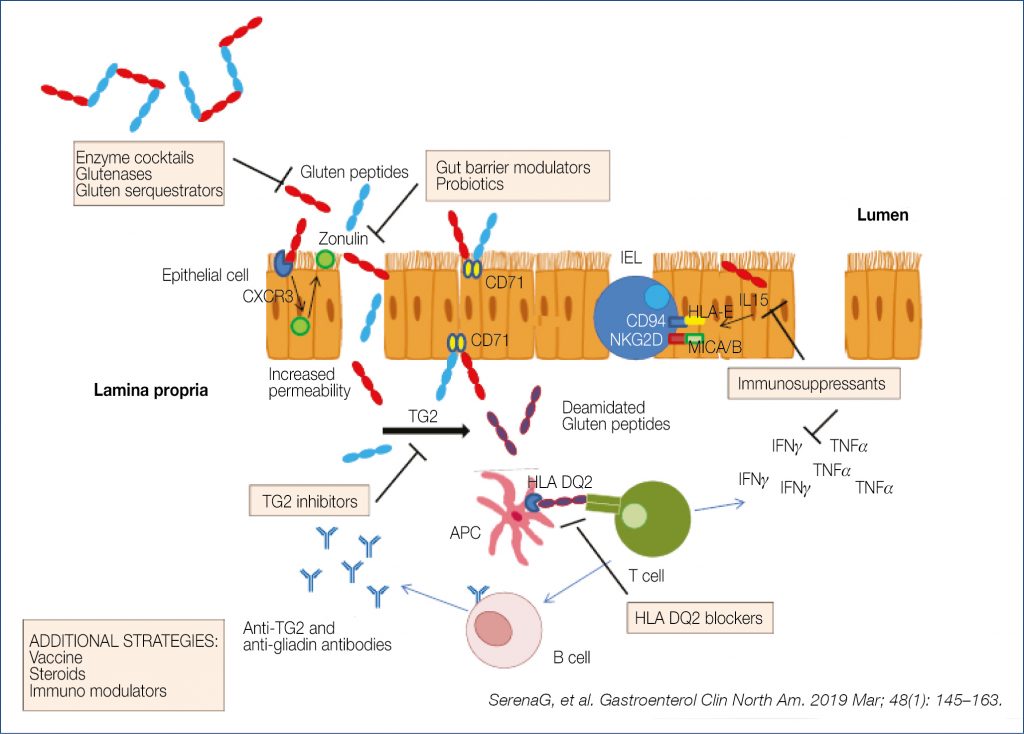
Hopefully some results of the many ongoing trials will lead to clinically useful application in the future. The American Gastroenterology Association recently published a clinical practice update on diagnosis and monitoring of celiac disease. What follows is a selection of the recommendations. High tissue transglutaminase (tTG-IgA) levels are reliable for diagnosing active disease. When celiac disease is suspected but biopsies are negative, positive tTG-IgA should lead to repeat biopsy sometime in the future. When patients have already started a gluten-free diet before a proper diagnosis was made, it is suggested that the patient goes back to a normal diet with three slices of wheat breaddaily for 1-3 months before repeat determination of tTG-IgA. A biopsy-avoiding diagnostic pathway was schematically suggested as shown in the figure below (Fig. 7).
Figure 7. AGA Clinical Practice Update on Diagnosis and Monitoring of Celiac Disease (6)
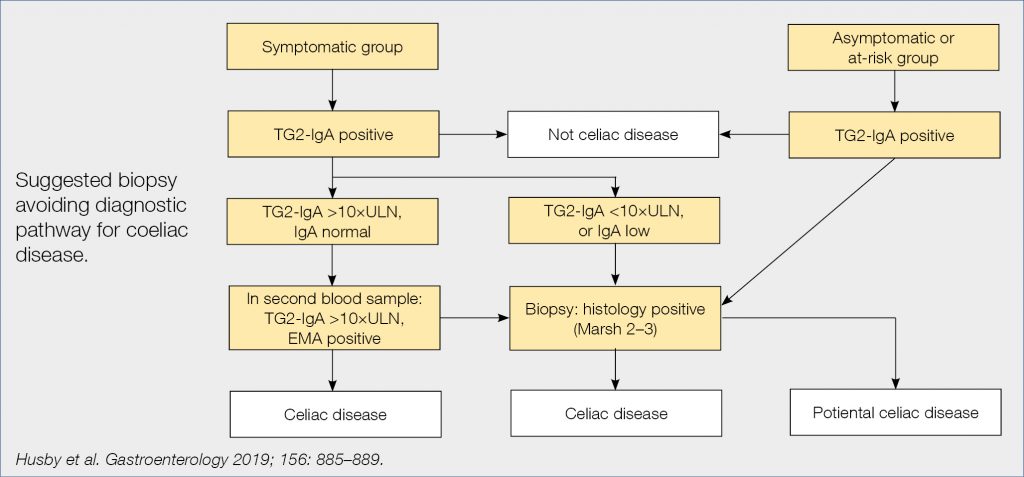
There is a rising interest for ‘point of care’ testing for several diseases, also for celiac disease with Simtomax, which detects IgA and IgG antibodies against deamidated gliadin peptides. This test was prospectively evaluated in over 1,000 German patients, of whom 4.1% had celiac disease. Simtomax’s sensitivity and specificity were respectively 79% and 94%, and positive and negative predictive value 37% and 99%, therefore unsuitable as a screening test in routineclinical practice.
Non-celiac gluten sensitivity, detected by controlled gluten challenge, may be present in a minority of all those avoiding gluten containing food (the gluten hype). Avoiding wheat products in such patients not only lowers the gluten intake but also the amount of FODMAPs, which may contribute to the symptom improvement. Yet a mild gluten-triggered immune reaction may also be ongoing in those sensitive individuals as suggested by higher numbers of intraepithelial CD3+ T-cells and lamina propria CD45+ cells and eosinophils in duodenal mucosa. More detailed studies are necessary before we understand the pathophysiological differences between celiac disease and gluten/wheat sensitivity.
Campylobacter jejuni is the leading cause of foodborne bacterial enteritis in humans. As shown in a large German study, consumption of chicken meat (74%) and eating out were the most important factors for campylobacter infection. Problematic is the rising antimicrobial resistance. In Japan, the ciprofloxacin resistance rose in ~10 y from 35% to 42%. Also in a Turkish cohort, campylobacter isolates were found to be resistant to ciprofloxacin (74%), tetracyclin (25%) and erythromycin (6%). In a French cohort, quinolone resistance rose from 48% to 55%. These are alarming figures making erythromycin or azithromycin now the treatment of choice. Prevention is crucial and only possible by meticulous avoiding of food contamination via raw chicken meat during food preparation.
Also non-typhoidal salmonella bacteremia is increasing especially in the elderly, as shown in a recent British study. Note that 34% of the bacteremia isolates were resistant to a first-line antibiotic regimen, frequently quinolone. Death occurred in 12% of the (most often) elderly patients. Other studies also pointed to the steady rise of plasmid-mediated quinolone resistance in human non-typhoidal salmonella infections.
The frequency of clostridioides difficile (a gram-positive, spore-forming anaerobic bacterium) is increasing worldwide. The infection may lead to severe life-threatening (pseudomembranous) colitis. The most important risk factors include antibiotic therapy, old age and hospital stay. Diagnosis is based on toxin detection in stool. Toxin A is an enterotoxin damaging the mucosal barrier function and stimulating intestinal secretion, and toxin B is a cytotoxin-driving inflammation. Antibiotic therapy of choice is based on vancomycin, fidaxomicin and, less so, metronidazole. In severe or recurrent or refractory patients, fecal microbiota transplantation may be successful in >90%. In successfully treated patients, a rapid and sustained stool enrichment was seen with microorganisms producing a bile salt hydrolase. This hydrolase converts taurocholic acid, a potent trigger for C. difficile germination, to cholic acid and deoxycholic acid, potent inhibitors of C. difficile growth. New British Society of Gastroenterology guidelines include the following statements:
- sterile 0.9% saline should be considered as an appropriate diluent for fecal transplant production and cryoprotectant, such as glycerol should be added for frozen preparations;
- >50 g stool, should be used per transplant preparation – stool should be mixed 1:5 with diluent to make the emulsion;
- homogenisation and filtration of the preparation should be undertaken in a closed disposable system.
More than 30 million individuals worldwide are yearly affected by traveller’s diarrhea. For prophylaxis, bismuth subsalicylate may be considered for any traveler, and rifaximin (but not fluoroquinolones) when antibiotic prophylaxis is indicated. The illustration below summerizes recent overall recommendations for traveller’s diarrhea (Fig. 8).
Figure 8. Recent overall recommendation for traveller’s diarrhea (7)
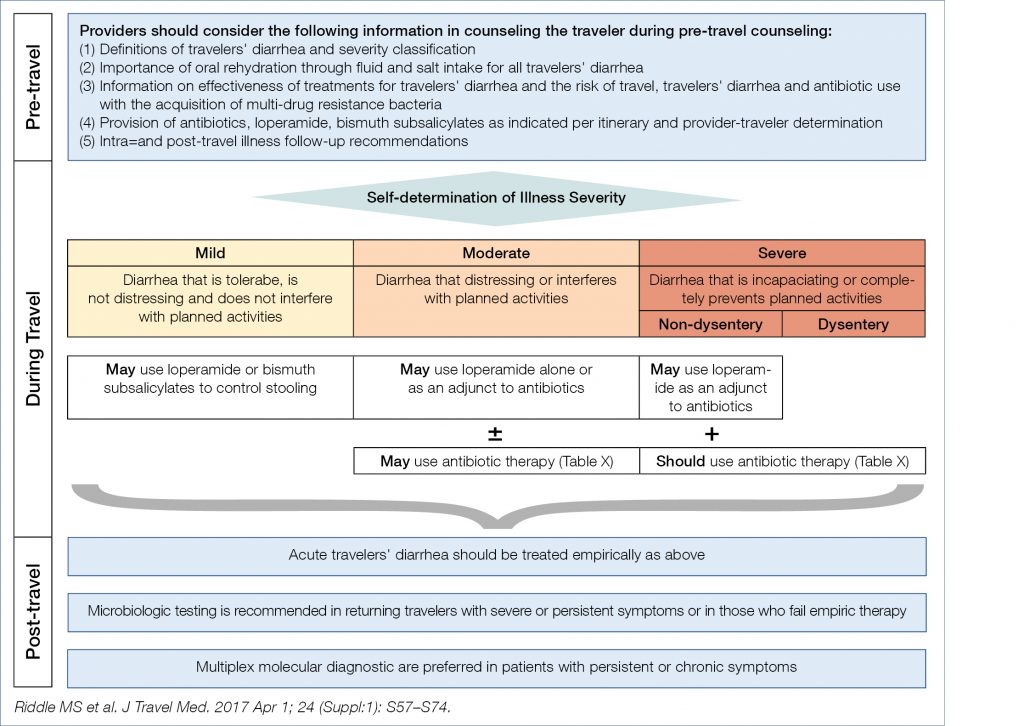
For moderate disease, both azithromycin (preferably a single dose) and rifaximin may be considered. Rifamysin SV-MMX is a novel poorby absorbed broad spectrum antibiotic, active against an-/aerobic,gram-pos/neg pathogens and shown to be as effective as ciprofloxacin, without substantial induction of extended-spectrum beta-lactamase-producing Escherichia coli.
Novel large bowel developments
Prof Jaroslaw Regula
Colorectal cancer is increasing worldwide, also in Europe where incidence and mortality were analysed from 1990 to 2016 in over 140 million people (20 countries) of whom over 180,000 had colorectal cancer diagnosed. The cancer incidence increased for the age group (20–29 y) by almost 8% (30–39 y) by almost 5% and (40–49 y) by 1.6%. The young-onset colorectal cancer was mainly due to rectal cancer in white individuals. Such puzzling rise in young-onset colorectal cancer could also be seen in population-based registries from several high-income countries, showing a decreasing incidence in people aged 50–74 y, but an increasing incidence in the 20–49 y old group. One can only speculate what the reasons could be for this distressing phenomenon: obesity causing smoldering inflammation? Microbiome changes due to antibiotic use? Inappropriate western-style diet? Food contaminants? Radiation exposure? More frequent predisposing genetic abnormalities? Other reasons? The question was even raised in the literature, whether the more frequent early-age onset should require lowering the starting age for screening, but so far relevant guidelines remained unchanged.
Many studies have shown the colorectal cancer preventive activity of acetylsalicylic acid. Whether another anti-platelet agent, clopidogrel, was also cancer preventive was analysed in a large Spanish nested case-control study, involving over 15,000 colorectal cancers and 60,000 randomly matched controls. When drug use was longer than one y, the adjusted Odds Ratio for acetylsalicylic acid was 0.79 and for clopidogrel 0.65. Why clopidogrel may decrease the incidence of colorectal cancer is unknown. The well-known and generally accepted prophylactic activity of acetylsalicylic acid was seriously questioned by the shocking results of a recent American study, involving close to 20,000 people above 70 y, comparing a low dose of 100 mg/d versus placebo for the duration of ~4.7 y. In the acetylsalicylic acid group the hazard ratio’s for
- all-cause mortality was (1.14);
- overall cancer related death (1.31);
- and colorectal cancer-related death (1.77).
Why the drug was not helpful in preventing colorectal cancer in the elderly and why it even shortened overall survival was unexpected, puzzling and shocking, and begs for confirmation and explanation!
Whether a healthy lifestyle is useful in colorectal cancer prevention was studied in over 40,000 patients compared to over 3,000 controls. The healthy lifestyle score was derived from five modifiable lifestyle factors: smoking, alcohol consumption, diet, physical activity, and body fatness. The genetic risk score was based on 53 known risk variants, based on genome-wide association studies. The higher the lifestyle score, the lower the cancer risk, independently of the genetic risk score. It is not known whether the mentioned lifestyle factors are of equal importance but regular physical activity seems important as also shown by other studies. Also diet is important as shown in the nurses/ health professionals follow-up study involving over 120,000 participants. Based on questionnaires the consumed diet pattern was classified as pro-inflammatory or as anti-inflammatory. Interestingly, the pro-inflammatory diet increased the risk of Fusobacterium nucleatum positive colorectal cancers. Presumably the pro-inflammatory diet altered the intestinal microbiome, favoring the outgrow of F. nucleatum, shown also in other studies to be commonly associated with colorectal cancer.
A novel quality metric to measure the impact of organised screening for colorectal cancer was recently proposed. The method is based upon the determination of the proportion of colorectal cancers, detected either by:
- screening;
- non-adherence (due to non-existing or non-adherence to existing screening programs);
- or interval cancers (screening done but cancer arose before the next recommended control).
An example of this metric may be seen in a recent American study. Of 572 cancers, 34.4% were screen detected 59.4% non-adherent and 6.1% interval cancer. Such metric data can now be compared between centers to evaluate and compare the screening efficacy. Obviously, the percentage screen-detected should be as high as possible and the percentage of interval cancers as low as possible. In real life it turns out to be quite difficult to lower the interval percentage, explaining the ongoing search for methods to improve the neoplasia detection rate during endoscopy. As pan-chromo-endoscopy is not very appealing for many colonoscopists, a variant was developed adding methylene blue MMX to the polyethylene glycol bowel prep solution, leading to more uniform colonic staining. Adding 200 mg methylene blue MMX versus placebo was evaluated in a multicenter controlled trial involving over 1,200 patients. The overall results are summerized in the figure below (Fig. 9).
Figure 9.The overall results (8)
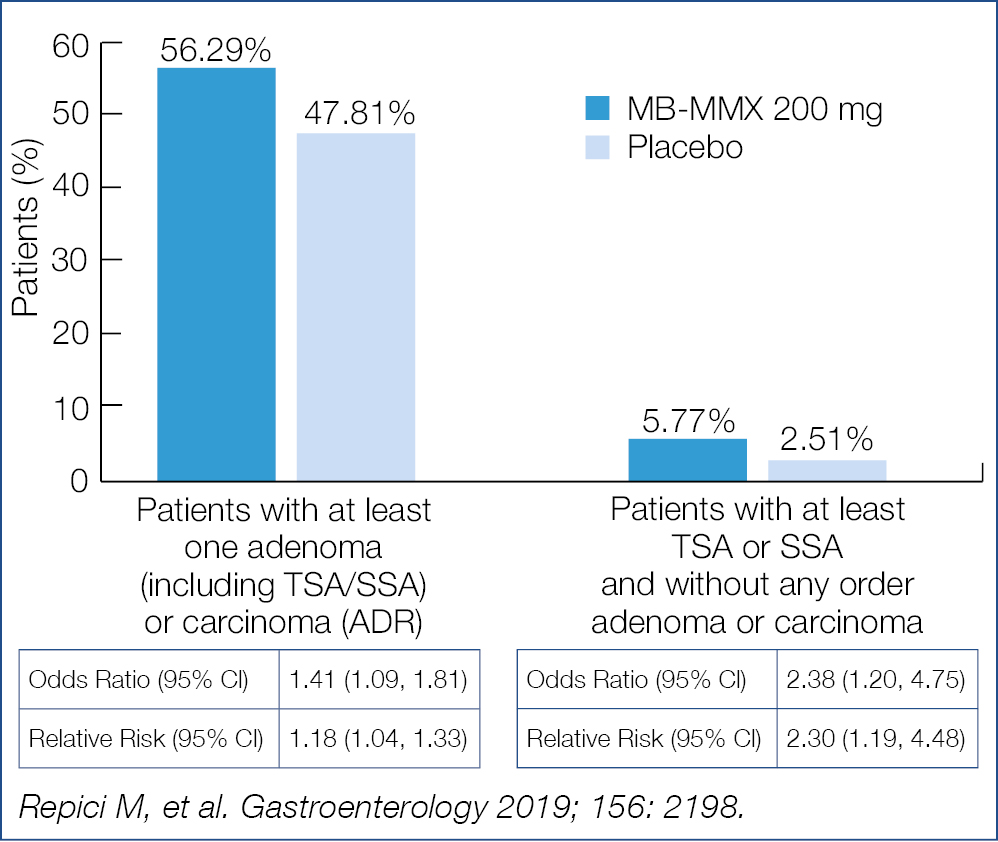
Methylene blue MMX added to the bowel prep significantly increased the adenoma detection rate. Whether this method will become the standard for screening requires further study.
Chronic use of acetylsalicylic acid or anticoagulants (warfarin or DOACs) is common in screening. Whether they interfere with Fecal immunochemical testing (FIT) for occult blood loss is somewhat controversial in the literature. To find out if FIT testing is reliable in users of those drugs, the positive predictive value was evaluated in 4,908 Norwegian individuals, including 1,008 acetylsalicylic acid users, 147 warfarin users and 212 DOAC users. The positive predictive value both for cancer and for advanced adenoma was significantly lower in the acetylsalicylic acid and DOAC users. Both patients and providers need to take note of this information when analysing the FIT results. The mechanisms explaining the phenomenon remain to be explored.
Not covered at the meeting but worthwhile mentioning are several recent data stressing the importance of additional ablation of the resection margins after colorectal polyp resection or the inclusion of an extra few mm of normal mucosa when cold resection is used to decrease the neoplasia recurrence rate, which may range up to 30% after removal of large flat lesions.
Symptomatic uncomplicated diverticular disease (SUDD) is a new disease entity, the pathophysiology of which is poorly understood. Indeed some 20% of patients with colonic diverticulosis develop symptoms without obvious signs of inflammation. To differentiate SUDD from IBS may be challenging. Using biopsies from the diverticular area compared to distant sites, immunochemical investigations revealed accumulation of macrophages in the peridiverticular mucosa. Nerve fiber sprouting was increased only in the diverticular region in SUDD patients, suggesting a role in symptom generation. The cause of these subtle mucosal alterations remains enigmatic but currently there is high research interest for mucosal interaction with the microbiome. In the same line is the interest in the efficacy of long-term rifaximin treatment (800 mg/d/7 d every month) for 8 y, as studied in 346 Italian SUDD patients compared to 470 similar patients, treated on demand by other means. There was significant improvement with rifaximin in the score for pain and bloating and stool frequency. These are intriguing results, begging for confirmation and for clarification of the underlying mechanism.
Novel pancreatic developments
Prof Peter Layer
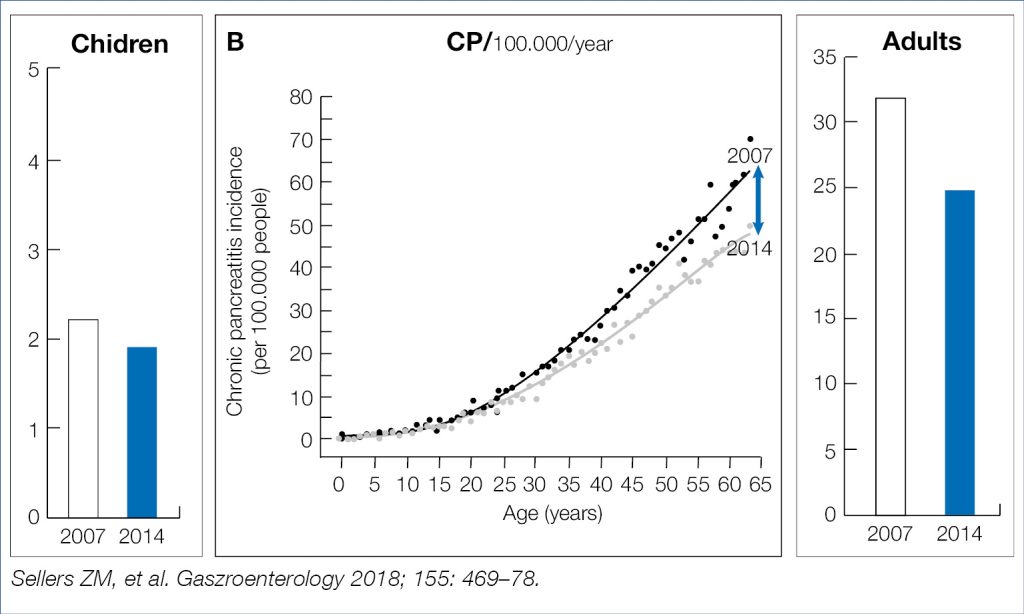
The steadily rising incidence over the previous decades of acute and chronic pancreatitis, presumably related to alcohol and tabacco consumption, obesity and cholelithiasis, was recently shown in a large American insurance data base to decline in adults, but not in children, as shown in the figures below (Fig. 10, Fig. 11). If this decline is related to decreasing nicotine consumption or increasing endoscopic/surgical obesity treatment remains speculative.
Figure 10. AP: Decreasing incidence in Adults (9)
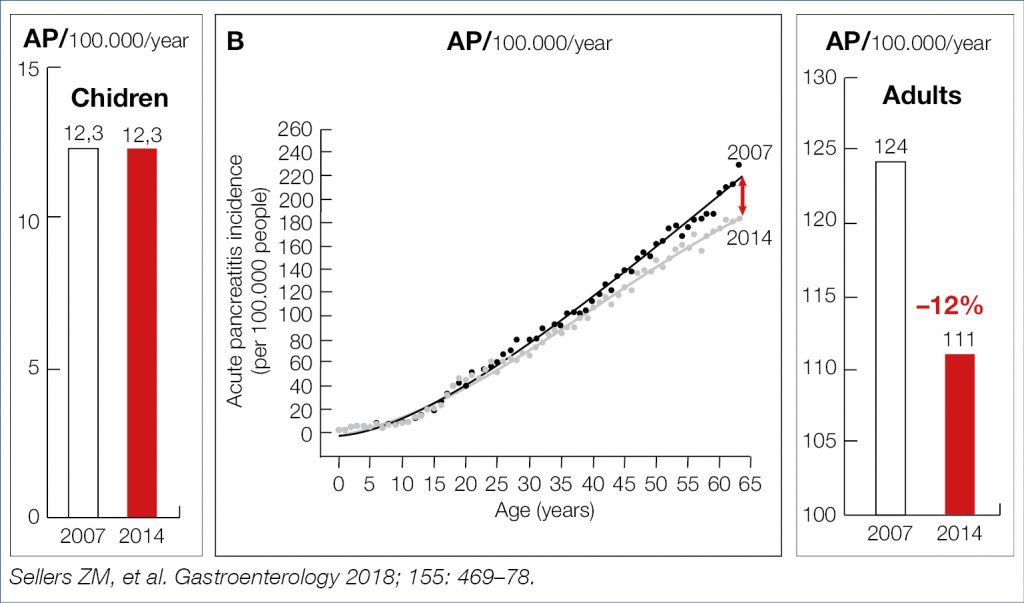
Figure 11. CP: Decreasing incidence in Adults (9)
Eluxadoline, a mixed opioid receptor modulator, available in some European countries for diarrhea-predominant irritable bowel syndrome, was shown in a post-marketing surveillance, to be responsible for inducing acute pancreatitis in over 16% of the adverse events compared to less than 1 % for all other anti-diarrheals (related to sphicter of Oddi dysfunction?). This would demand a re-evaluation of eluxadoline’s benefit-hazard ratio.
Ramadan, celebrated by Muslims, includes dawn-to-dusk fasting, followed by an opulent evening meal which may lead to massive gall bladder contractions, perhaps favoring gall stone mobilization with risk of pancreatitis. Indeed the risk of acute pancreatitis was shown to be 2.5 times higher during the Ramadan month. Following prolonged fasting, massive nutritive stimulation may lead to vigorous contraction of a distended gall bladder, to rapid increase in serum triglycerides and glucose and to massive stimulation of pancreatic enzyme secretion. Ramadan followers should be advised to break the fast gradually, especially if cholelithiasis is present.
A simple cheap and particularly rapid prognostic marker in acute pancreatitis is the neutrophil-to-lymphocyte ratio in peripheral blood. The normal ratio is ~1.65. A value >10 was shown to predict high severity of acute hypertriglyceridemia-induced pancreatitis, with prolonged hospital stay, enhanced risk for SIRS and renal failure. These exciting data warrant further prospective evaluation in all forms of acute pancreatitis.
Acute pancreatitis is often associated with nausea, vomiting, gastrointestinal hypomotility and subileus, conditions favoring bacterial overgrowth, bacterial translocation and infectious complications. Bacterial overgrowth, studied by a (poorly sensitive) glucose breath test at day 7 in over 200 pancreatitis patients, was demonstrable
in over 25% of the patients with a severe cause and with organ complications. Early enteral feeding, whenever feasible, would presumably lead to early stimulation of gastrointestinal motility and reduction of intestinal stagnation and bacterial overgrowth.
Healing of acute pancreatitis may be associated with irreversible structural and functional deficits. The prevalence of exocrine pancreatic insufficiency was evaluated some 36 m after the acute attack in a meta-analysis involving almost 1,500 patients. Exocrine insufficiency was present in one quarter of the patients, particularly in patients with alcoholic pancreatitis or with a severe necrotizing course. Clinicians should be on the outlook for insufficiency during follow-up. Unfortunately an easy simple (stool) test, also sensitive for minor degrees of insufficiency, is still not available.
Over the last few years, a paradigm shift has occurred with respect to the management of acute necrotising pancreatitis. Early emergency surgery (often open necrosectomy) is obsolete and initial management should be conservative. If surgical intervention should be necessary it should be selective, late-elective and leading to minimal trauma. Minimally invasive surgery led to a 20–30% lower mortality compared to open necrosectomy. Also endotherapy in high risk patients had a 60–79% lower mortality compared to open necrosectomy. Optimal management of severe acute pancreatitis with infected necrosis requires an individually adapted minimally invasive strategy. If interventions are needed, endoscopic methods are less traumatic and produce overall better results compared with minimally invasive surgery. This was again confirmed in a recent study, showing that endoscopic therapy when performed in experienced centers by experts is safe and cost-effective. The main reasons for endoscopic superiority was a lesser occurrence of enteral or pancreatic-cutaneous fistulae and lower rate of systemic inflammatory response syndrome.
Chronic pancreatitis is a dreadful condition. Alcohol and smoking has a deleterious influence on the natural evolution as shown by a ~10 y follow-up study comparing alcoholics (75% smokers) to non-alcoholics (<40% smokers). Chronic pain, pseudocysts, pancreatitis flares, exocrine insufficiency, and number of hospitalisations were significantly higher in the alcoholic cohort. Stressing the need to abstain from alcohol and to stop smoking remains of high clinical relevance. Intriguing is the impact of statins on the natural evolution of chronic pancreatitis, as shown in a population based cohort of close to 5,000 patients of whom 43% died and 2.4% developed pancreatic cancer. Overall mortality, disease progression and pancreatic cancer risk were lower in statin users. Statin use may be associated with protective (anti-fibrogenetic, anti-carcinogenetic) effects in chronic inflammatory diseases such as chronic pancreattis. Intraductal papillary mucinous neoplasia (IPMN) may occasionally lead to cancer, particularly when involving the main pancreatic duct. Many use the Fukuoka criteria to estimate the cancer risk, looking for – worrisome features (WF) (pancreatitis, cyst >3 cm, thickened or enhanced cystic wall, main pancreatic duct >5 mm, non-enhanced cyst mural nodule, abrupt change in main pancreatic duct caliber with distal atrophy) and high-risk stigmata (HR) (obstructive jaundice, solid components with enhancement, main pancreatic duct >10 mm). European guidelines were recently published regarding the diagnostic and therapeutic management of IPMN as shown below (Fig. 12).
Figure 12. Diagnostic and Therapeutic Management of IPMM: European Guidelines (10)
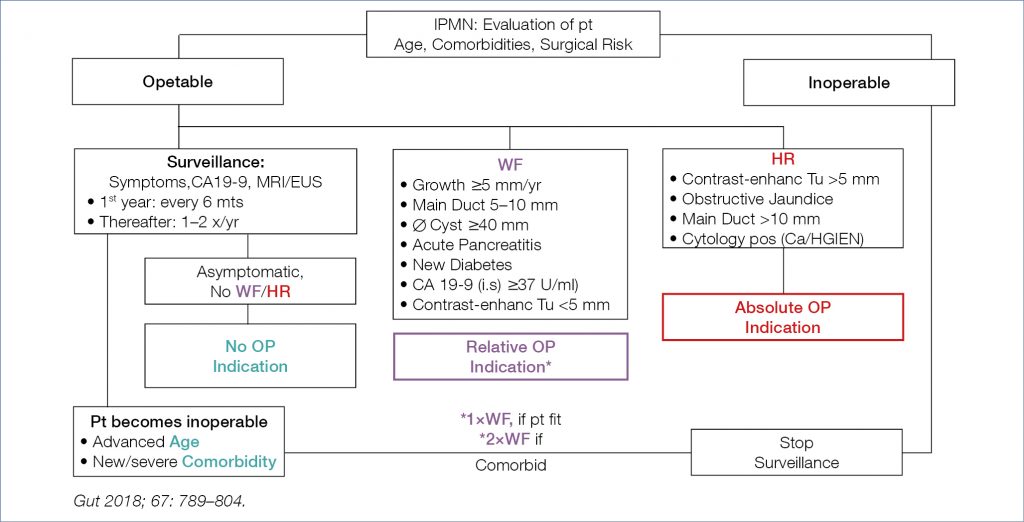
Based on several new studies following main recommendations conclusions can be drawn:
- IPMNs, even if initially Fukuoka negative, are (and become) never “safe”. Therefore, long-term surveillance ( >5 y ) is warranted, as long as the patient is fit for surgery;
- initial cyst size alone is not a worrisome feature per se but predicts later development of worrisome features, as does also occur for rapidly enlarging cysts by >2.5 mm/y
For cysts of an indeterminate nature, measuring glucose in the cyst fluid may offer a simple, quick, cheap and precise diagnostic marker for its neoplastic nature. This was shown in a study of over 150 resected cystic lesions of various subtypes. Cyst glucose was substantially lower in the mucinous type cysts compared to non-mucinous cysts. Using a glucose cut-off value of 50 mg/dl, the accuracy of the glucose test was 90% compared to 69% for CEA determination with a cut-off at 192 ng/ml.
Cyst ablation may be attempted in high risk IPMN in patients unfit for pancreatic surgery by EUS-guided instillation of cytostatic drugs (gemcitabine and paclitaxel) dissolved in alcohol or saline respectively. Complete cyst ablation at 12 m was obtained in respectively 61% and 67%, with severe 30 d adverse events in 6% versus 0% and mild 30 d adverse events in 22% versus 0%. These results need to be confirmed in other studies with long-term follow-up before this method becomes standard therapy.
Pancreatic cancer remains the number one dismal conundrum in gastroenterology. For many years, prevention has been suggested by drugs such as acetylsalicylic acid and vitamin D. Disappointingly the large long-term American nurses/ health professionals study revealed that both drugs offered no relevant protection against pancreatic cancer. As biomarkers for early disease are not yet available, we are left to be on the outlook for early symptoms. Newly diagnosed diabetes may be the first symptom of an underlying pancreatic malignancy. This was nicely shown in 219 cancer cases versus 440 controls. As shown in the figure below (Fig. 13), hyperglycemia may be observed as early as 30–36 m prior to cancer diagnosis. The degree of blood glucose elevation correlated with both the tumor size and degree of undifferentiation.
Figure 13. Diabetes mellitus as early symptom of pancreatic carcinoma (11)
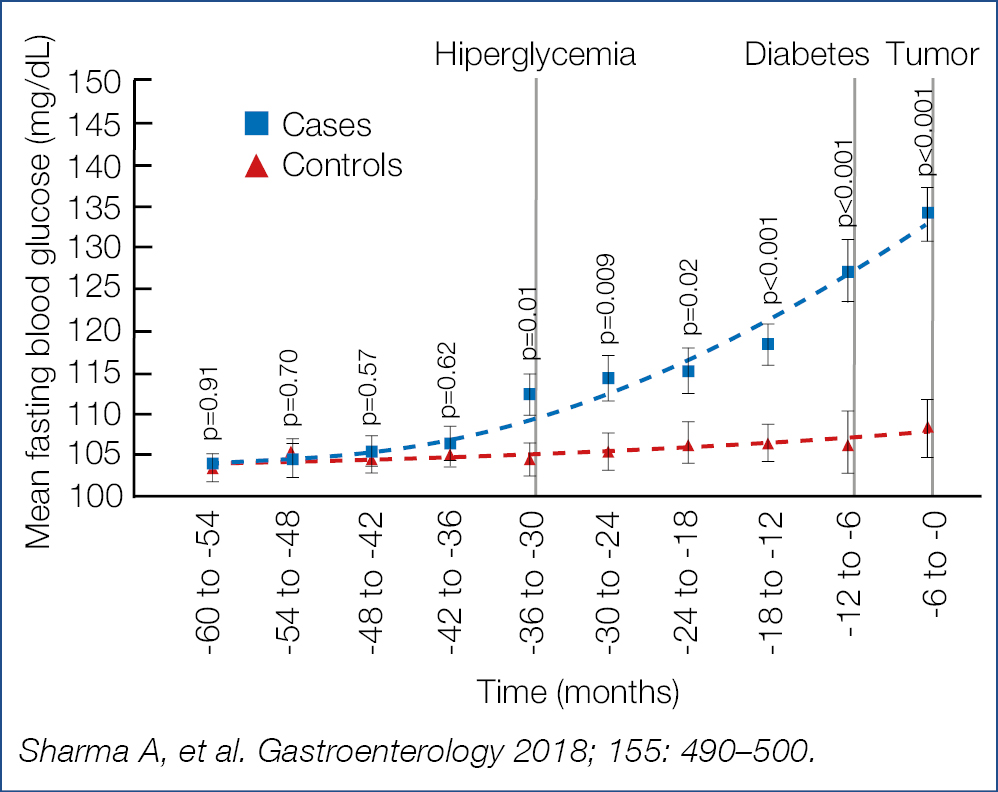
Development of pancreatic cancer points to complex interactions with the metabolism of glucose, with chronic hyperglycemia favoring neoplasia. Therefore, in all patients with new-onset of diabetes, particularly when associated with preceding weight loss, increased vigilance is mandatory and, as a rule, abdominal ultrasound is warranted.
Novel developments in intestinal endoscopy
Prof Oliver Pech
Most western studies on endoscopic resection of early esophageal malignancy are related to adenocarcinoma. Now a new French multicenter study with long-term follow-up of endoscopic resection of 148 squamous cell cancers was presented, 54% treated with mucosal resection and 46 % treated with submucosal dissection. Median lesion size was 20.5 mm; 38% were piece-meal resected; depth of cancerous infiltration was (m 1-2) in 64% and (m3-sm) in 36%; the procedure was complicated by bleeding in 2%, perforation in 2% and led to stricturing in 14%. During a median follow-up of 22 months, tumor recurrence was observed in 14.2%. Significant risk factors for recurrence, expressed as hazard ratios were: –removal by mucosal resection (17) – pT1m3-sm (3) – need for additional chemoradiotherapy (7) – non-curative resection (12). If at all possible piece-meal resection should be avoided and for larger lesions or suspicion for submucosal ingrowth, submucosal dissection is to be preferred. Radiofrequency ablation of early sqamous cancer has also been evaluated in 35 Chinese patients. Complete response was seen in 86%. Tumor recurrences were observed in 20% but could all be treated with endoscopic resection. Meticulous examination of the resection specimens suggested that initial expansion of cancerous growth in the ductular epithelial lining of the submucosal glands, extending deeper than the muscularis mucosae and therefore not ablated, was the presumed cause of the cancerous recurrence.
Although it is commonly known that longstanding achalasia is a risk factor for squamous cancer, little is known about the impact of 3 yearly endoscopic screening with lugol staining as evaluated in a cohort of 230 patients followed for a median of 56 m after various treatments (pneumodilation, surgical myotomy, POEM,PPI etc.) Stasis of food or liquids was observed in 27% during 1 or more endoscopies. In ~a quarter of the endoscopies reflux esophagitis, usually grade A and B, was detected. Low grade dysplasia was detected in 3% and evolved into cancer in 1.3%, resulting in an overall incidence rate of sqamous cancer of 63/100,000 person-years. The incidence rate of low grade dysplasia started rising after 20 y of achalasia symptoms and cancer after 30 y of symptoms. Stagnant decomposing food and fluid and bacterial overgrowth, leading to chronic mucosal injury and inflammation, are considered to contribute to the oncogenic process and should be the leading target of the various therapies.
Studies continue to be published regarding the therapy with resection and/or usually radiofrequency ablation of neoplastic columnar metaplastic (Barrett) mucosa, confirming studies mentioned in previous highlights. Controversies remain whether patients should be intensively surveilled in the absence of any dysplasia or whether asymptomatic patients should be treated with non-stop PPI antisecretory treatment. Whether there are prognostic phenotypes for esophageal adenocarcinoma was prospectively evaluated in a separate American and British cohort. Interestingly the overall survival in both cohorts was substantially better when intestinal metaplasia was present in the peritumoral mucosa compared to those where intestinal metaplasia was absent. Thus adenocarcinoma without intestinal metaplasia appeared to have a significantly worse outcome. A confounder in the concept of two different types of esophageal adenocarcinoma is the fact that it is almost impossible to rule out overgrowth of intestinal metaplasia by aggressive tumor expansion. All this reminds the ongoing controversy regarding the requirement of intestinal metaplasia with goblet cells as a prerequisite for proper diagnosis of Barrett type columnar metaplasia.
Usually covered self-expanding metal stents are used for palliation of advanced esophageal carcinoma, largely to prevent cancerous ingrowth. The full covering however favors the risk of migration. Does it help to leave both ends of the stent uncovered? In a controlled Dutch trial, almost 100 patients were randomized to fully versus partially covered stents. No differences were found between the 2 stent types regarding technical success and frequency of recurrent obstruction. Recurrent obstruction was more frequent for proximal cancers.
Benign strictures usually respond to bougie/balloon dilation therapy but some are truly recalcitrant and recurrent. Is temporary stenting with a biodegradable stent with chronic dilation while tissue remodeling occurs helpful in such patients with recurrent benign esophageal strictures? In a controlled multicenter trial, 66 patients with esophageal strictures, most often anastomotic strictures, with prior dilation up to at least 16 mm were randomized. During the first 3 months significantly less repeat endoscopic dilations were necessary in the biodegradable stent grou, but significance was no longer seen at 6 months. The median time to the first re-dilation was longer in the stent group (106 d) versus the control group (42 d). There were 2 perforations in the control group versus 5 stent occlusions, 2 tracheoesophageal fistulas and 1 migration in the stent group. I am wondering what the proper indications (if any) are for biodegradable stenting and if radial incision with a needle-knife would not be a more attractive approach for anastomotic stricturing, realising however that no controlled comparative studies are available.
Bleeding in the upper gastrointestinal tract remains a challenge, particularly for recurrent bleeding of peptic ulcers. To find out whether over-the-scope (OTSC) clips are superior to standard therapy with clipping or coagulation, 66 patients were randomized in a multicenter study. Persistent bleeding or recurrent bleeding within 7 d was significantly lower in the OTSC group (15%) versus the control group (58%). Ulcer type, Forrest type, Rockall score, anticoagulation and type of prior endoscopic therapy had no significant impact. OTSC clipping requires adequate anatomic targeting of the bleeding area which may occasionally be challenging; perhaps monopolar hemostatic forceps may be helpful in such circumstances. A consecutive cohort of 112 Turkish patients with bleeding gastroduodenal ulcers were randomized to treatment with monopalar hemostatic forceps with soft coagulation versus hemoclipping. Hemostasis was obtained in respectively 98% versus 80% with a median of 3 clips. Monopolar hemostatic forceps was successful in all clip failures (persistent or recurrent bleeding within 7 d). Hemostatic forceps were more effective than hemoclips independent from ulcer and bleeding type. Other studies have confirmed the usefulness of hemostatic forceps in the treatment of acute bleeding.
Peroral endoscopic myotomy (POEM) has become the minimally invasive treatment of choice for achalasia in many centers. A well-documented adverse consequence is the high frequency and often severe nature of reflux disease, sometimes insufficiently controlled with acid suppressant therapy. Surgical Heller-type myotomy is often combined with partial (Dor-type) fundoplication. Is a comparable combination possible by endoscopic means? This was attempted in a rather provocative proof of concept study by Inoue, the inventor of POEM. Distal to the myotomy, the proximal stomach was perforated, allowing endoscopic entry into the peritoneal cavity, positioning of a large endoloop over de fundus, anchoring the most distal and proximal part of the loop with clips and final closing the loop creating a partial fundoplication. There were no complications and the plication appeared endoscopically detectable in almost all patients 2 m later. Obviously many questions remain to be answered but such attempt is a nice illustration of the ongoing exploration of novel therapeutic possibilities.
Using the submucosal tunnel space to approach the muscle layer is not limited to the esophageal sphincter. A logical extension was to cut the obstructing gastric pyloric sphincter complex, called G-POEM to ameliorate refractory gastroparesis. A meta-analysis of 7 studies, involving almost 200 such patients was presented. Clinical success was seen in 82% and the gastroparesis cardinal symptom index decreased significantly in parallel, with scintigraphic emptying studies. Obviously large controlled trials are required now to identify the subset of patients where this novel therapy would be most appropriate, also with long-term follow-up.
All endoscopists are aware of the difficulties in getting permanent optimal cleaning/desinfection of the endoscopic equipment. What is insufficiently realised is the risk of bacterial exposure of the face of the endoscopist during the procedure through exposure to blood and body fluids. Swabs of plastic face shields worn by the endosopist or positioned on the suite wall were cultured before and after the procedure. The number of bacterial colony forming units was low before the endoscopy but rose substantially post-procedure in 46% of the face shields worn by the endoscopists and in 21% hanging on the suite wall. Unrecognized face exposure occurs 5.6 times per 100 half-day endoscopic procedures and individuals standing up to 6 feet away from the patient may still be exposed at a rate of 3.4 per 100 half-day presence in the endoscopy suite. The authors of that study make a plea for routine face protection for the endoscopist and assisting staff. Uncleaned suite surfaces may aid in patient-to-patient transmission of pathogens.
A major drawback of endoscopic (mucosal) resection of usually large laterally spreading colonic adenomas is the high recurrence rate of up to 30%, especially after piece-meal resection, as discovered during surveillance after 3–6 m. Can thermal ablation of the resection margin reduce this high recurrence rate? This was investigated in a large multicenter controlled trial in Australia in laterally spreading lesions, more than 2 cm in diameter. Piece-meal resection was followed by snare tip soft coagulation of the entire resection margin (soft coag effect 4, 80 watts). Surveillance endoscopy, performed at 5-6 and 18 m, included meticulous inspection of the scar with white light and narrow band imaging with biopsies of the scar center and margin and of any suspicious area. Close to 400 patients with over 400 lesions were included. Endoscopic recurrence was observed in ~7% in the ablation arm versus ~21% in the control arm, and histologic recurrence in respectively ~5% versus ~23%. Endoscopic assessment had a sensitivity of ~92%, a specificity of ~97% and a negative predictive value of ~99% for correctly identifying recurrence at the post-resection scar. The value of ablation of the margins has now been confirmed in other studies. Even in studies evaluating the usefulness of cold snare resection, the advice is usually given to include a generous surrounding tissue margin to decrease the risk of local recurrence.
A remaining challenge for endoscopists is the detection of deep submucosal cancerous invasion in polypoid lesions. Up to now, T1 colorectal polyps with one or more risk factors for lymph node metastasis are considered endoscopically unresectable. Can narrow band imaging (NBI) be helpful in identifying deep malignant invasion? A large multicenter prospective Spanish study explored the usefulness of NBI in over 1,600 patients with well over 200 polyps larger than 1 cm. Pointers for deep invasion were – brown/dark brown discoloration with/without whiter patches -areas of disrupted/missing vessels – amorphous/absent surface pattern. Of the lesions 4.2% had features of deep invasion and 4.3% were considered endoscopically unresectable. The NBI – based prediction of deep malignant infiltration had a sensitivity 58%, a specificity of 96% and a positive and negative predictive value of respectively 42% and 98%. Beyond a doubt such results are encouraging but there is still room for improvement. We live certainly in exciting times, now that experts are exploring removal of (well differentiated) rectal lesions extending up to the muscularis propria by dissecting the plane between the circular and longitudinal muscle. The endoscopic boundaries keep moving.
Biliopancreatic endoscopy
Prof Marco Bruno
Developments in endoscopic ultrasound (EUS), biliopancreatic endoscopy and endoscopic complications were discussed. Microbial contamination of endoscopic equipment remains a major (unsolvable?) problem for the endoscopist. Over the past 17 y, 32 documented duodenoscope-related outbreaks with multi-drug resistant microorganisms, involving over 400 patients and leading to death in over 20 patients, have been reported. Endoscopic contamination and patient infection have also occurred without breaches in the re-processing procedures. Scope contamination after a procedure is ~8-10 log10; manual cleaning leads to a reduction with ~4-6 log10 and further automated high level disinfection to another ~4-6 log10 reduction. The total reduction amounts to ~8-12 log10 leading to a low margin of safety of ~0-2 log10. Sratches and shredding in bending sections and remaining adherent debris interfere with the cleaning/disinfection efficacy. These results were again confirmed in a nation-wide duodenoscope culture study, showing that 22% of the duodenoscopes were contaminated with one or more microorganisms with 20 or more colony forming units and that 39% of the ERCP centers had at least 1 contaminated duodenoscope hanging in the dryer cabinet. Contamination was not confined to a specific duodenoscope type but appeared related to the complex scope design and the inability to sufficiently clean all its intricate surfaces. A recent American FDA safety communication reads: For high concern organisms, defined as organisms that are more often associated with disease, such as E. coli and Pseudomonas aeruginosa, updated culturing results appear to show that up to 5.4% of properly collected samples test positive. Combined with strict adherence to the duodenoscope manufacturer’s reprocessing instructions, the following supplemental measures may further help reduce the risk of infection transmission associated with the use of duodenoscopes:
- microbiological culturing;
- ethylene oxide sterilization;
- use of a liquid chemical sterilant processing system;
- repeat high-level disinfection. Perhaps the last recommendation is the most sensible and realistic or shall we be using only disposable (duodeno)endoscopes in the not-to-distant future?
In a previous large scale Dutch controlled trial, a minimally invasive step-up approach was shown to be superior at a follow-up of 6 m, to primary open surgical necrosectomy in patients with (infected) necrotizing pancreatitis. The endpoint (mortality/major complications) was respectively 40% versus 69%. Recently, the late outcome after ~ 86 m was superior for the step-up approach with significantly less new-onset multi-organ failure/systemic complications, incisional hertnia and need for pancreatic enzyme therapy. Lumen-apposing metal stents are increasingly being used in the drainage of pancreatic walled-off necrosis instead of plastic pig-tail stents. A recent meta-analysis showed a comparable overall clinical success rate of 88% with both modalities. Also the difference in pooled adverse event rates of respectively 11% versus 16% was not significant, leaving the choice to the endoscopist’s preference. The overall similar outcomes between expandable metal versus pig-tail plastic was again shown in a British study with comparable technical and clinical success (above 90%), stent duration of an average 55 d and recurrence rates of around 5-6%. What was different was the higher rate of bleeding, 15% versus 3%, with about half the bleeding in the metal stent cohort related to the development of a pseudo-aneurysm, necessitating vascular embolization. Other publications have drawn attention to this dreadful aneurysmal complication, caused by excessive pressure trauma of vessels in the wall of the necrotic cavity by the expandable metal stents. Patients should be prewarned of such potential complications.
Quite revolutionary is the rapidly spreading experience with EUS-guided gastrointestinal connections mainly for palliation of malignant obstruction. In one such study, EUS-guided choledocho-duodenostomy was carried out in 46 patients with inoperable malignant distal bile duct obstruction. Technical and clinical success was respectively 93% and 98%. Adverse events occurred in 12% (stent food impaction, delayed bleeding and stent migration). Reaching the papilla for ERCP can be challenging, for example after gastric bypass surgery with Roux-en-Y anastomosis for therapy of morbid obesity. Reaching the papilla may be attempted with a balloon-fitted endoscope. Alternatively, the gastric pouch may be reconnected transmurally under EUS guidance. In a multicenter study, EUS-guided gastrogastrostomy was compared with endoscopy in 60 patients. Technical success by reaching the papilla was seen in 100% versus 60% with a procedure duration of 50 min versus 91 min, both in favor of the EUS-guided approach. Adverse effects were comparable with 10% and 7%. Several comparable studies, evaluating the efficacy of the EUS-guided transintestinal approach have been published, all indicating comparable technical and clinical success rates and comparable and sometimes even lower complication rates when compared to other modalities, such as percuteous transhepatic approches etc.
Also intriguing is the exploration of the usefulness of cholangioscopy now that the digital single-operator cholangioscope has become available. This technology was evaluated in a multicenter study with over 400 patients with difficult biliary stones, defined as
- >15 mm,
- >3,
- intrahepatic/cystic duct, and/or – impacted or – associated with anatomic duct abnormality.
Complete bile duct clearance, either with electrohydrolic or laser lithotripsy was obtained in 97%, in 1 session in 77%. ERCP’s for additional therapy such as stent removal or stricture treatment was necessary in 34%. The most important factor associated with technical failure was difficult anatomy or difficult cannulation. More than one session was more often necessary in patients with prior failed ERCP or in case of a prolonged initial cholangioscopy session. Current guidelines suggest cholangioscopy-guided lithotripsy as an adjunct with or without balloon dilation or mechanical lithotipsy. Novel is the evaluation of direct cholangioscopy guided laser lithotripsy. Endoscopic stone clearance was obtained in respectively 93% and 67% of the 60 patients. Dilation of the papilla was more often carried out in the conventional group and the procedure duration was substantially longer in the cholangioscopy group. The conventional approach was less successful in patients with prior ERCP attempt. The usefulness of cholangioscopy was also demonstrated for biopsy targeting of suspicious lesions, yet distinguishing between benign and malignant bile duct stricturing lesions often remains challenging. Whole exome and genome sequencing studies have defined the genetic landscape of neoplasms arising or secondarily involving the bile duct system. A 28-gene next-generation-sequencing panel (BiliSeq) was prospectively evaluated in 346 ERCP-obtained biliary specimens from 252 patients with bile duct strictures. The sensitivity and specificity of BiliSeq for malignant strictures was respectively 73% and 100%. In comparison, the sensitivity of elevated serum CA 19-9 was 76% and of pathological evaluation 48%. The combination of BiliSeq and pathological evaluation increased the sensitivity to 83% and maintained a specificity of 99%. BiliSeq improved the pathological sensitivity for both biliary brushings and biopsies. Among patients with primary sclerosing cholangitis, BiliSeq had a sensitivity of 83% compared to 8% or pathological examination. Interestingly, in 8% the genomic alterations were useful in guiding therapy such as trastuzumab-based treatment for ERBB2-amplified cholangiocarcinoma. Beyond doubt, increasingly molecular-based investigations will be incorporated in diagnostic/therapeutic endoscopy.
The explosive interest in pancreatic cysts has continued during the past year.The overall subtyping of cystic lesion is illustrated below (Fig. 14).
Fine needle aspiration cytology was the standard technology when trying to characterize the nature of the cystic lesion but attention is increasingly switching to the use of newly designed catheter-guided biopsy needles.
Figure 14. Pancreatic Cysts. What are we looking for? (12)
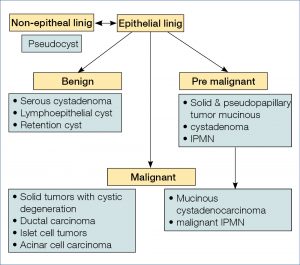
Novel is the development of catheter-guided microbi-opsy forceps for targeted biopsy of the cystic wall. In 28 patients the micro-biopsy procedure was technically successful in 86%. Biopsies were generally of good quality and contributed to the diagnosis in over 70%. Adverse events occurred in 11%, usually mild pancreatitis. Such results were confirmed in another cohort of 56 patients where the procedure was technically successful in all. Mild adverse events were seen in 16%, most commonly intracystic bleeding. Specimens were considered adequate for histology in 84%, leading to an overall diagnostic accuracy, combining histology and cytology of 84%. What the proper and cost-effective indications will be for use of micro-biopsy forceps equipment needs further larger scale detailed multicenter evaluation.
These narrative highlights cover only part of the lectures presented at the Gastro Update Europe 2019 meeting in Budapest. Not covered in this review are hepatology, oncology, neuromotility, surgery and the exciting case presentations. These highlights intend to illustrate the high educational level of the meeting, emphasizing the most important developments in gastroenterology – hepatology of relevance for the practicing specialist. This type of compact and comprehensive update can be recommended for both fellows and astute practitioners in our discipline.
The Gastro Update Europe 2020 will be held on June 5 – 6, 2019 in Bratislave, Slovakia (Vienna Airport). For more information visit www.gastro-update-europe.eu
2. Hunt RH, Scarpignato C. Curr Treat Options Gastroenterol 2018 Dec; 16(4): 570–590. https://doi.org/10.1007/s11938-018-0206-y
3. Adapted Malfertheiner et al Nat Rev Gastroenterol and Hepatol 2017; 14(12): 697–710. https://doi.org/10.1038/nrgastro.2017.117
4. 5 O’Shea KM, Aceves SS, Dellon ES, Gupta SK, Spergel JM, Furuta GT, Rothenberg ME. Gastroenterology 2018 Jan; 154(2): 333–345. https://doi.org/10.1053/j.gastro.2017.06.065
5. Serena G, et al. Gastroenterol Clin North Am 2019 Mar; 48(1): 145–163. https://doi.org/10.1016/j.gtc.2018.09.011.
6. Husby, et al. Gastroenterology 2019; 156: 885–889. https://doi.org/10.1053/j.gastro.2018.12.010.
7. Riddle MS, et al. J Travel Med 2017 Apr 1; 24(suppl 1): S57–S74. https://doi.org/10.1093/jtm/tax026.
8. Repici M, et al. Gastroenterology 2019; 156: 2198. https://doi.org/10.1053/j.gastro.2019.02.001.
9. Sellers ZM, et al. Gastroenterology 2018; 155: 469–78. https://doi.org/10.1053/j.gastro.2018.04.013
10. European Study Group on Cystic Tumours of the Pancreas. Gut 2018 May; 67(5): 789–804. https://doi.org/10.1136/gutjnl-2018-316027
11. Sharma A, et al, Gastroenterology 2018; 155: 490–500. https://doi.org/10.1053/j.gastro.2018.04.025
12. Marco Bruno – Gastro Update Europe 2019.
